Why the Coronavirus Has Been So Successful
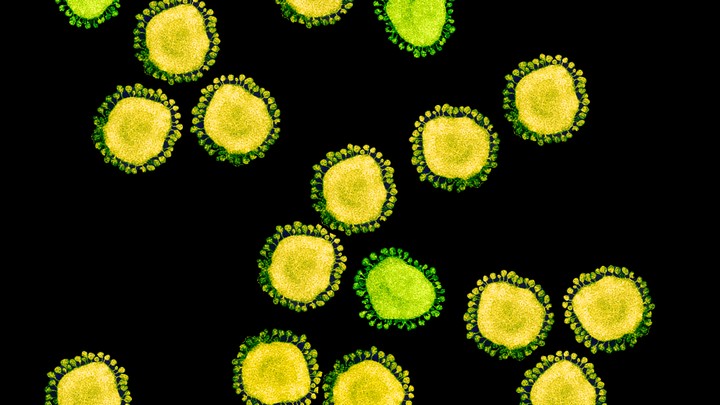
One of the few mercies during this crisis is that, by their nature, individual coronaviruses are easily destroyed. Each virus particle consists of a small set of genes, enclosed by a sphere of fatty lipid molecules, and because lipid shells are easily torn apart by soap, 20 seconds of thorough hand-washing can take one down. Lipid shells are also vulnerable to the elements; a recent study shows that the new coronavirus, SARS-CoV-2, survives for no more than a day on cardboard, and about two to three days on steel and plastic. These viruses don’t endure in the world. They need bodies.But much about coronaviruses is still unclear. Susan Weiss, of the University of Pennsylvania, has been studying them for about 40 years. She says that in the early days, only a few dozen scientists shared her interest—and those numbers swelled only slightly after the SARS epidemic of 2002. “Until then people looked at us as a backward field with not a lot of importance to human health,” she says. But with the emergence of SARS-CoV-2—the cause of the COVID-19 disease—no one is likely to repeat that mistake again.
To be clear, SARS-CoV-2 is not the flu. It causes a disease with different symptoms, spreads and kills more readily, and belongs to a completely different family of viruses. This family, the coronaviruses, includes just six other members that infect humans. Four of them—OC43, HKU1, NL63, and 229E—have been gently annoying humans for more than a century, causing a third of common colds. The other two—MERS and SARS (or “SARS-classic,” as some virologists have started calling it)—both cause far more severe disease. Why was this seventh coronavirus the one to go pandemic? Suddenly, what we do know about coronaviruses becomes a matter of international concern.
The structure of the virus provides some clues about its success. In shape, it’s essentially a spiky ball. Those spikes recognize and stick to a protein called ACE2, which is found on the surface of our cells: This is the first step to an infection. The exact contours of SARS-CoV-2’s spikes allow it to stick far more strongly to ACE2 than SARS-classic did, and “it’s likely that this is really crucial for person-to-person transmission,” says Angela Rasmussen of Columbia University. In general terms, the tighter the bond, the less virus required to start an infection.
MORE STORIES
There’s another important feature. Coronavirus spikes consist of two connected halves, and the spike activates when those halves are separated; only then can the virus enter a host cell. In SARS-classic, this separation happens with some difficulty. But in SARS-CoV-2, the bridge that connects the two halves can be easily cut by an enzyme called furin, which is made by human cells and—crucially—is found across many tissues. “This is probably important for some of the really unusual things we see in this virus,” says Kristian Andersen of Scripps Research Translational Institute.
For example, most respiratory viruses tend to infect either the upper or lower airways. In general, an upper-respiratory infection spreads more easily, but tends to be milder, while a lower-respiratory infection is harder to transmit, but is more severe. SARS-CoV-2 seems to infect both upper and lower airways, perhaps because it can exploit the ubiquitous furin. This double whammy could also conceivably explain why the virus can spread between people before symptoms show up—a trait that has made it so difficult to control. Perhaps it transmits while still confined to the upper airways, before making its way deeper and causing severe symptoms. All of this is plausible but totally hypothetical; the virus was only discovered in January, and most of its biology is still a mystery.
The new virus certainly seems to be effective at infecting humans, despite its animal origins. The closest wild relative of SARS-CoV-2 is found in bats, which suggests it originated in a bat, then jumped to humans either directly or through another species. (Another coronavirus found in wild pangolins also resembles SARS-CoV-2, but only in the small part of the spike that recognizes ACE2; the two viruses are otherwise dissimilar, and pangolins are unlikely to be the original reservoir of the new virus.) When SARS-classic first made this leap, a brief period of mutation was necessary for it to recognize ACE2 well. But SARS-CoV-2 could do that from day one. “It had already found its best way of being a [human] virus,” says Matthew Frieman of the University of Maryland School of Medicine.
This uncanny fit will doubtlessly encourage conspiracy theorists: What are the odds that a random bat virus had exactly the right combination of traits to effectively infect human cells from the get-go, and then jump into an unsuspecting person? “Very low,” Andersen says, “but there are millions or billions of these viruses out there. These viruses are so prevalent that things that are really unlikely to happen sometimes do.”
Since the start of the pandemic, the virus hasn’t changed in any obviously important ways. It’s mutating in the way that all viruses do. But of the 100-plus mutations that have been documented, none has risen to dominance, which suggests that none is especially important. “The virus has been remarkably stable given how much transmission we’ve seen,” says Lisa Gralinski of the University of North Carolina. “That makes sense, because there’s no evolutionary pressure on the virus to transmit better. It’s doing a great job of spreading around the world right now.”
Read: The U.K.’s coronavirus “herd immunity” debacleThere’s one possible exception. A few SARS-CoV-2 viruses that were isolated from Singaporean COVID-19 patients are missing a stretch of genes that also disappeared from SARS-classic during the late stages of its epidemic. This change was thought to make the original virus less virulent, but it’s far too early to know whether the same applies to the new one. Indeed, why some coronaviruses are deadly and some are not is unclear. “There’s really no understanding at all of why SARS or SARS-CoV-2 are so bad but OC43 just gives you a runny nose,” Frieman says.
Researchers can, however, offer a preliminary account of what the new coronavirus does to the people it infects. Once in the body, it likely attacks the ACE2-bearing cells that line our airways. Dying cells slough away, filling the airways with junk and carrying the virus deeper into the body, down toward the lungs. As the infection progresses, the lungs clog with dead cells and fluid, making breathing more difficult. (The virus might also be able to infect ACE2-bearing cells in other organs, including the gut and blood vessels.)
The immune system fights back and attacks the virus; this is what causes inflammation and fever. But in extreme cases, the immune system goes berserk, causing more damage than the actual virus. For example, blood vessels might open up to allow defensive cells to reach the site of an infection; that’s great, but if the vessels become too leaky, the lungs fill even more with fluid. These damaging overreactions are called cytokine storms. They were historically responsible for many deaths during the 1918 flu pandemic, H5N1 bird flu outbreaks, and the 2003 SARS outbreak. And they’re probably behind the most severe cases of COVID-19. “These viruses need time to adapt to a human host,” says Akiko Iwasaki of the Yale School of Medicine. “When they’re first trying us out, they don’t know what they’re doing, and they tend to elicit these responses.”
During a cytokine storm, the immune system isn’t just going berserk but is also generally off its game, attacking at will without hitting the right targets. When this happens, people become more susceptible to infectious bacteria. The storms can also affect other organs besides the lungs, especially if people already have chronic diseases. This might explain why some COVID-19 patients end up with complications such as heart problems and secondary infections.
But why do some people with COVID-19 get incredibly sick, while others escape with mild or nonexistent symptoms? Age is a factor. Elderly people are at risk of more severe infections possibly because their immune system can’t mount an effective initial defense, while children are less affected because their immune system is less likely to progress to a cytokine storm. But other factors—a person’s genes, the vagaries of their immune system, the amount of virus they’re exposed to, the other microbes in their bodies—might play a role too. In general, “it’s a mystery why some people have mild disease, even within the same age group,” Iwasaki says.
Coronaviruses, much like influenza, tend to be winter viruses. In cold and dry air, the thin layers of liquid that coat our lungs and airways become even thinner, and the beating hairs that rest in those layers struggle to evict viruses and other foreign particles. Dry air also seems to dampen some aspects of the immune response to those trapped viruses. In the heat and humidity of summer, both trends reverse, and respiratory viruses struggle to get a foothold.Read: How you should get food during the pandemic
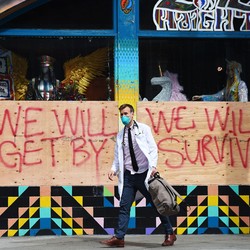
Unfortunately, that might not matter for the COVID-19 pandemic. At the moment, the virus is tearing through a world of immunologically naive people, and that vulnerability is likely to swamp any seasonal variations. After all, the new virus is transmitting readily in countries like Singapore (which is in the tropics) and Australia (which is still in summer). And one recent modeling study concluded that “SARS-CoV-2 can proliferate at any time of year.” “I don’t have an immense amount of confidence that the weather is going to have the effect that people hope it will,” Gralinski says. “It may knock things down a little, but there’s so much person-to-person transmission going on that it may take more than that.” Unless people can slow the spread of the virus by sticking to physical-distancing recommendations, the summer alone won’t save us.
“The scary part is we don’t even know how many people get normal coronaviruses every year,” Frieman says. “We don’t have any surveillance networks for coronaviruses like [we do for] flu. We don’t know why they go away in the winter, or where they go. We don’t know how these viruses mutate year on year.” Until now, research has been slow. Ironically, a triennial conference in which the world’s coronavirus experts would have met in a small Dutch village in May has been postponed because of the coronavirus pandemic.
“If we don’t learn from this pandemic that we need to understand these viruses more, then we’re very, very bad at this,” Frieman says.


/media/img/mt/2020/03/0320_Pinsker_Martin_Family/original.png)

No comments:
Post a Comment